Dynamical Properties of Postural Control in Obese Community-Dwelling Older Adults
Does obesity affect balance and serve as an indicator of fall risk in this vulnerable population?
Excerpt By Thurmon E. Lockhart
The burden of obesity is rising at an alarming rate for older adults. The prevalence of obesity (BMI >30 kg/m2) is higher in older adults aged 60 and over (37%) than in younger adults5 and is associated with risk factors for various health conditions (e.g., cardiovascular diseases, stroke and diabetes). Obese individuals also have higher chances of sustaining injuries compared to their lean counterparts. Falls were identified as the most common cause of injury (36% of all injuries) in obese adults and obese older adults fell almost twice as frequently (27%) as their lean counterparts (15%).
Although epidemiological studies clearly link increased fall risk to obesity in older adults, the mechanism through which obesity increases falls and fall risk is unknown. Indeed, an array of obesity-related physiological and biomechanical factors induce postural/gait alterations that may increase fall risks. For example, obesity is associated with an anteriorly displaced center of mass (COM) and influences trunk posture while standing and walking, which may impair static and dynamic stability. Obesity may also influence the development or progression of a wide variety of musculoskeletal conditions that may influence body movement and postural stability,17,18 leading to more falls. Furthermore, additional postural and gait-control constraints associated with obesity are largely unidentified and their role unknown.
This article has been excerpted from Frames CW, Soangra R, Lockhart TE, et al. Dynamical Properties of Postural Control in Obese Community-Dwelling Older Adults,” which appeared in Sensors; 2018;18:1692. References have been removed for brevity. Use is per the Creative Commons Distribution 4.0 International License. To read the full article, go to https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6021983/
In this study, to quantify the dynamical properties of postural stability, several nonlinear measures, expressed as time series of center of pressure (COP) trajectories in both force plate and inertial measurement units (IMU), were employed. These measures were anticipated to provide further insights into postural control mechanisms associated with obesity. In order to improve accessibility of routine analysis of gait and posture in assessing fall risk of an individual, a wearable wireless accelerometer-based gait and postural analysis system (along with the traditional force plate) was employed.
Dynamic postural control, defined as the ability to maintain equilibrium despite the presence of small disturbances or control errors, is a fundamental motor task that must be rapidly adapted in the face of a dynamically varying environment. Within physiological systems, variability from internal and external stressors is often synonymous with error. However, over the past three decades, focus has shifted from the amount of variability in the system to the time-dependent structure of variability to represent the system’s global health. Using a dynamical systems theoretical framework, it has been reported that physiological systems are inherently complex and nonlinear in nature. A variety of mathematical analyses have been developed since then to calculate how the system dynamics change throughout the lifespan or due to pathology.
Within system dynamics, the loss of complexity hypothesis was introduced, which suggested as adults age, the complexity of their dynamics decreases. In the years following, the loss of adaptability and optimal movement variability models were developed with a bidirectional consideration, suggesting that too little or too much complexity reflects a less adaptive system.51 These new models bridged the observations supporting the loss of complexity hypothesis while also explaining the increased complexity observed in certain tasks and populations. With these conceptual frameworks in mind, researchers have generally interpreted the degree of complexity within system dynamics as indicative of its adaptive capacity—a reflection of the system’s global health.
The aim of this study was to determine if obesity affects balance in community-dwelling older adults and serves as an indicator of fall risk.
Methods
Ninety-eight community-dwelling older adults (mean age 74.3±7.6 years) participated in the study. This sample size was selected to provide a smaller confidence interval on the estimated error rate when classifying fallers and non-fallers.36 Study participants were divided into three groups based on their BMI: normal (19≤BMI<25 kg/m2), overweight (25≤BMI<30 kg/m2), and obese (30≤BMI<40 kg/m2).36 Fall history was recorded retrospectively for two years with emphasis on frequency and characteristics of the falls. Any person with at least one fall in the prior year was classified as a faller and the others as non-fallers.
The study was conducted in four separate community centers throughout Virginia using the same set of instruments (IMU and force plate) on four different days. All measurements were performed barefoot in quiet standing, looking in the forward direction, with foot placement standardized. Participants were asked to stand in two visual conditions: eyes open (EO) and eyes closed (EC). Each measurement lasted for 60 seconds and was repeated twice. The sampling rate was 100 Hz. A rest of three minutes was provided between each measurement.
Key Findings
- Postural and gait stability is compromised in obese fallers.
- Acceleration-based gait and postural parameters are able to distinguish between obese fallers and non-fallers.
Discussion
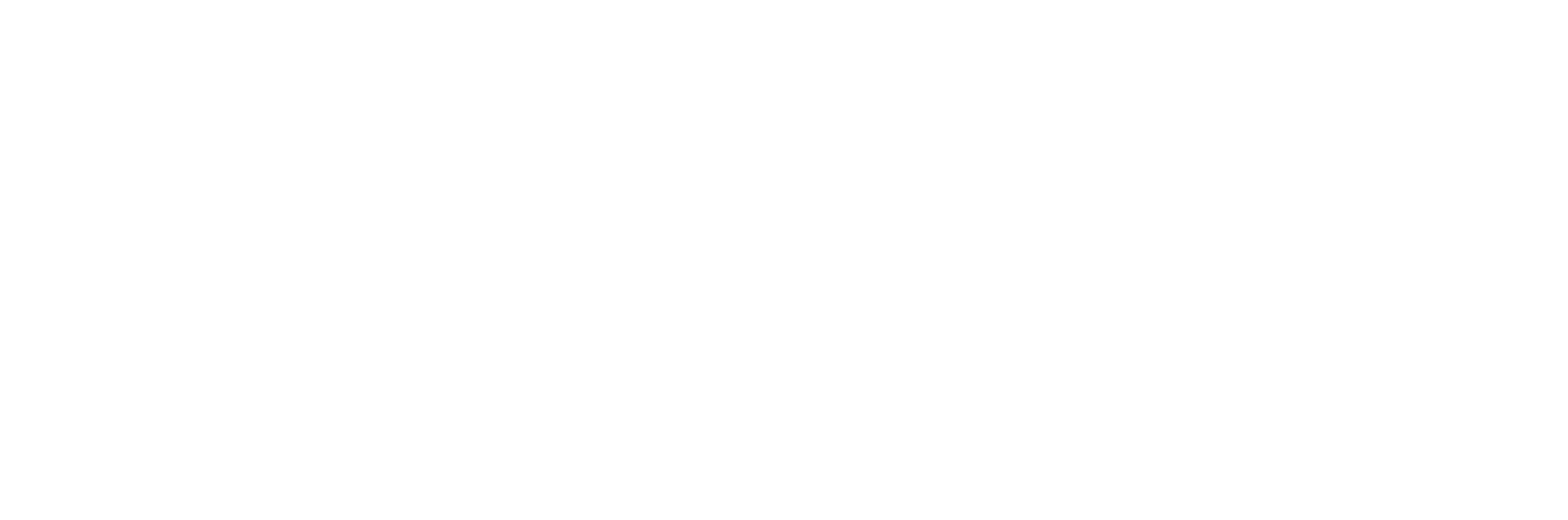
This study investigated the effects of obesity on fall risk in community-dwelling older adults, utilizing nonlinear analyses on signals acquired from force plate and IMU measurements. A significant increase in linear parameters (mean radius, ellipse area, sway range, root mean square [RMS], standard deviation [SD]) was identified for obese older adults. Nonlinear regularity measures through multiscale entropy revealed that the presence of obesity and fall risk had a loss of complexity (Figure 1).
In the present study, entropy-based estimations of organizational variability delineate the adaptive capacity of obese participants to maintain balance. Obese older adults were found to have significantly lower approximate entropy (ApEn) and sample entropy (SaEn) values during prolonged quiet standing in the anterior-posterior (AP) direction, indicating greater regularity and possibly decreased complexity. The findings coincide with previous investigations37 linked with the theory of decreased complexity attributed to pathology and aging.47 Bodily degrees of freedom are constrained in the AP direction compared to the medio-lateral (ML) direction, whereby coordination of the physiological system, coupled with environmental stressors, lead behavioral processes into less complex, more stable response modes—a more regular sway pattern with closed-loop short-term dependencies to restore balance. The motor system is unable to adjust to the demands inherent to obesity; therefore, movements transition to a more rigid postural-control behavior (repeated patterns and decreased complexity) in the AP direction that diminish both adaptability and stability. In this context, the increase in regularity and possible decrease in complexity may be a result of impaired feedback control or impaired proprioception leading to a reduced adaptive capacity of the postural system.
FACILITIES AND OTHER RESOURCES
 The Locomotion Research Labortory is located at the Physical Education Building East (PEBE) on the campus of Arizona State University at Tempe. The two-story building has office and collaboration spaces. The building features two laboratories, preparation or/ changing rooms, three conference rooms, numerous graduate student offices and student workstations. The shared-use facilities utilize more than 2000 sq. ft. of space that is configured for the development of rehabilitation technology and for neuromotor assessment in individuals with disabilities.
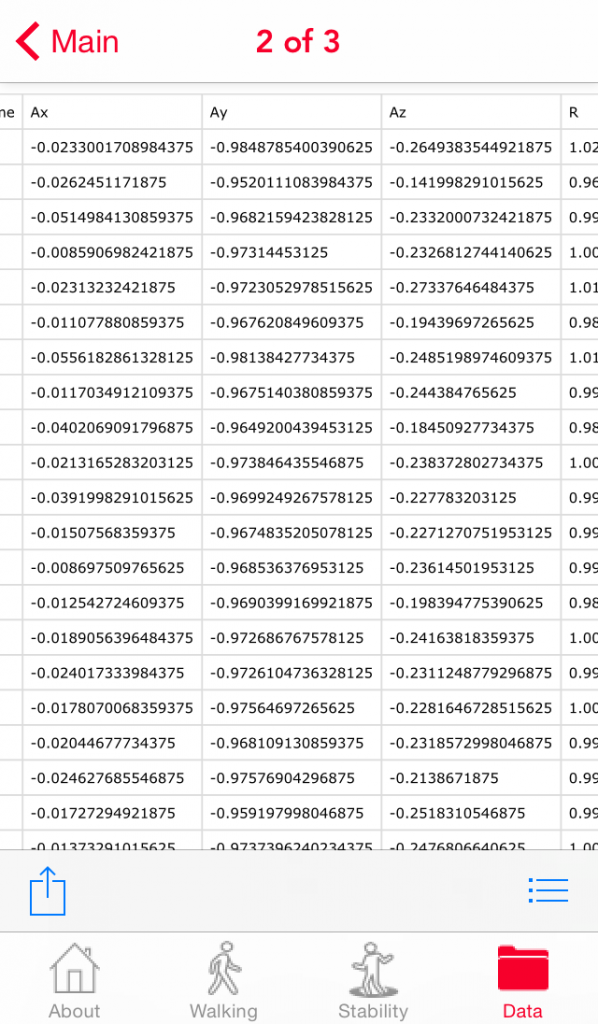
The Locomotion Research Labortory is located at the Physical Education Building East (PEBE) on the campus of Arizona State University at Tempe. The two-story building has office and collaboration spaces. The building features two laboratories, preparation or/ changing rooms, three conference rooms, numerous graduate student offices and student workstations. The shared-use facilities utilize more than 2000 sq. ft. of space that is configured for the development of rehabilitation technology and for neuromotor assessment in individuals with disabilities. The laboratory has space and equipment to enable non-invasive measurements of biomechanical, neural control, metabolic and cardiorespiratory variables. The facility includes a gait lab that is equipped for kinematic and kinetic analysis of overground locomotion and has a ceiling-mounted low-friction harness system for safe perturbation experiments. One adjacent room houses the Motek Medical GRAIL system which consists of a dual-belt instrumented treadmill capable of delivering pitch, sway, and surge perturbations. The gait lab and the GRAIL treadmill space both have ceiling mounted harnesses for safety that also allow rigorous testing of situation when balance is compromised.
The laboratory has space and equipment to enable non-invasive measurements of biomechanical, neural control, metabolic and cardiorespiratory variables. The facility includes a gait lab that is equipped for kinematic and kinetic analysis of overground locomotion and has a ceiling-mounted low-friction harness system for safe perturbation experiments. One adjacent room houses the Motek Medical GRAIL system which consists of a dual-belt instrumented treadmill capable of delivering pitch, sway, and surge perturbations. The gait lab and the GRAIL treadmill space both have ceiling mounted harnesses for safety that also allow rigorous testing of situation when balance is compromised.

1) Gait Laboratory (approximately 20’ x 40’) – Only slightly smaller than the size of a basketball court with 24’ ceilings, this laboratory features two force plates (BertecCorporation), and Vicon Motion Analysis Corporation 3D digital motion capture system (10 cameras).
 2)Virtual Reality laboratory – A 43’ x 29’ laboratory housing a rear-projection Virtual Reality system that is integrated with 3 Video Cameras and 10-Bonita Infra-red cameras with Vicon 3D digital motion capture system, and a Bertec instrumented split-belt treadmill. In addition, a wireless Delsys EMG system synchronized using D-Flow software from Motek Medical.
2)Virtual Reality laboratory – A 43’ x 29’ laboratory housing a rear-projection Virtual Reality system that is integrated with 3 Video Cameras and 10-Bonita Infra-red cameras with Vicon 3D digital motion capture system, and a Bertec instrumented split-belt treadmill. In addition, a wireless Delsys EMG system synchronized using D-Flow software from Motek Medical.
Major Equipment for the proposed project:
The Locomotion Research Labortory has all the equipment needed for the successful completion of various biomechanical projects. The Lab includes state-of-the-art laboratory equipment for virtually any biomechanics project available. All equipment is housed within the PEBE hall and the PI has immediate access to all equipment. Equipment specific to this project includes
following instruments:
– 3D motion-capture system: (VICON®, nexus, 3 video cameras and 10 Bonita camera, Oxford Metrics, Oxford, UK) that tracks the kinematics of whole body movement within the integration of kinetics. It can also provide real time (10ms delay) feedback to the kinematics of the markers.
– Instrumented split-belt treadmill: ; a dual-belt instrumented treadmill (GRAIL, Motek Medical BV, Amsterdam) with pitch (incline/decline), sway (medial/lateral), and surge (anterior/posterior) capabilities, immersive real-time video, and kinematic tracking; other treadmills.
– Xsens is 3D motion tracking technology and its sensor fusion technologies enable a seamless interaction between the physical and the digital and 3D character animation and motion analysis. Three Awinda stations for cahrginag and wireless transmission. The Awinda Station can receive data from up to 20 MTw’s simultaneously Data from multiple MTw’s is time-synchronized to within 10μs Charges up to 6 MTw’s simultaneously.
– Trigno™ Wireless Systems and Smart Sensors: 16 EMG channels, 48 accelerometer channels with 16-bit resolution, 1926 Hz EMG sampling rate with 8 hours of operation in full transmission mode.
– Jamar Grip Strength Dynamometer measures isometric grip force from 0–200 lbs (90 kg).
– AMTI’s AccuGait Optimized™ multi-axis force platform is a portable forceplate for quantifying human gait and balance. The AccuGait’s forceplate is accurate, economical, and easy to use with AMTI’s powerful NetForce software. It has plug & play USB interface which automatically synchronizes multiple platforms and eliminates external power supplies. AccuGait Optimized has unprecedented levels of accuracy for measuring Center of Pressure, forces and moments, as well as dramatic reductions in crosstalk.
How to Fall On Your Butt without Breaking Your Neck
The right way to fall, according to science
Follow these four rules, and increase your odds of having a safe landing.
1. Walk Like You’re on a Tightrope
Whether you’re traversing an icy parking lot or a slick office floor, your best defense against a fall is a good defense.
Make slow, short steps, and extend your arms out to your sides, like you’re walking across a tightrope.
Doing this helps maintain you balance, and it positions your arms closer to where they’ll need to be to save you if things go south. And speaking of . . .
2. Use Your Arms
Let’s say your feet slip and you begin falling backwards. You’re going to feel helpless, and your first instinct is probably to flail your arms wildly, looking for something to grab onto or to cushion your body.
You’ll have better luck with a more decisive move: Fling your arms forward and up, so your center of gravity moves forward. This may be enough to stabilize you.
If that doesn’t work, it’s time to . . .
3. Bring Your Arms to Your Side
Everything in your body will scream, ”Cushion the fall with your hands!” It’s a natural instinct to think you can somehow catch yourself before you hit the ground. Isn’t that what they do in all the martial arts movies?
You should resist that instinct. Instead, lower your arms to your sides. Especially if you’re falling backwards. That’s how guys end up breaking their wrists.
Related: 20 Little Changes For a Healthier Life
If your arms are at your side, that’s what will hit the ground first, before your hips. And that’s exactly what you want.
Wrists and hips break far too easily. Your arms will fare much better, especially if you tense up before the impact. Tense muscles protect ligaments and bones.
Related: Try the 21-Day MetaShred—the Cutting-Edge Fat-Loss System That Will Banish Your Belly and Build Rock-Hard Muscle
4. Try to Land on Your Butt
If you can help it, land flat on your rear.
And then, in a single, smooth motion, roll onto your hip—the one opposite your slipping leg—to help diffuse the force of the fall.
If you’re falling forward and there’s no way of directing your fall towards your ass, try to fall into a pushup position.
You’ll avoid a nasty head (or face) injury, and your bent elbows will reduce impact on your wrists.
http://www.menshealth.com/health/right-way-to-fall
Canes, walkers linked to higher risk of falls By Janice Neumann
Walkers and canes can be lifesavers for older people, but a new study highlights the downside of using them without training.
“A lot of older adults seem to struggle with their walking aids . . . they often drag along their walking aids like a burden with a difficult gait pattern as a result, possibly increasing the risk of falling,” said the study’s lead author, Tine Roman de Mettelinge of Ghent University in Belgium.
Older people need to be able to function independently, but gait problems can undermine that, even leading to nursing home admission, Roman de Mettelinge and her coauthor point out in the Journal of Geriatric Physical Therapy.
The study followed 43 adults, ages 63 to 94, in a residential care facility in Belgium. Twenty-two used walking aids (most used a four-wheeled walker, two used a two-wheeled walker, one used a walker without wheels and one used a cane).
Researchers tracked their falls, as well as factors that might have contributed to the accidents, such as cognitive problems, fear of falling, use of psychotropic drugs or age.
They also measured residents’ muscle strength, walking speed, and how much their arms were swinging as they moved.
Altogether, 22 residents (15 using walking aids and seven not using walking aids) had at least one fall.
After accounting for psychotropic drug use, falls in the previous years, older age, slower walking, longer periods spent standing still and less arm swinging, people who used walking aids were still nearly four times more likely to fall than those who did not.
Those who fell walked much more slowly and took smaller steps than those who did not fall.
“A substantial proportion of the relationship between using walking aids and future falls” could be explained by altered gait, older age and use of psychotropic drugs, Roman de Mettelinge said in an email. The factors with the greatest effect seemed to be cadence, stance and swing percentage, she added.
Such results are “common knowledge to many researchers,” said Thurmon E. Lockhart, a professor in the School of Biological and Health Systems Engineering at Arizona State University, who called the study “very, very important.”
But the take-home message isn’t as simple as avoiding walking aids, said Lockhart, who was not involved in the study.
“It gives kind of a mixed message but the bottom line is the device in itself may not cause future accidents, but at the same time since there’s a relationship between fall risk and the device use, we need to watch out for that a little in the future,” he said.
While a cane might help with mobility, it could also make it more difficult for people to stabilize themselves during a fall, Lockhart noted.
“It’s almost all about how we recover” from loss of balance, he said.
Lockhart has developed a “slip simulator,” where an individual walks on a shifting linoleum floor controlled by a computer. The person wears a harness and learns to regain a sense of balance as the floor shifts.
“They’re learning about themselves, about their limits of balance and stability . . . the only way to train that is to slip and fall,” Lockhart said.
Roman de Mettelinge said doctors and therapists should consider an individual’s physical and mental abilities and living conditions before prescribing a walking aid.
Someone who needs a walking aid should be given balance and gait exercises and then be trained to safely use a walker or cane, including proper gait patterns and ways to avoid falls, she said. The training should also include complicated maneuvers like opening and closing doors with the aid.
Roman de Mettelinge cautioned that the results of the study applied to individuals in assisted care facilities, who tend to be older and in poorer health than people still living at home.
SOURCE: bit.ly/1DFzuhD Journal of Geriatric Physical Therapy, online January 15, 2015.
<http://mobile.reuters.com/article/idUSKBN0LA21G20150206>
Preventing Slips, Trips and Falls
Get Inside the Science:
- Virginia Tech: Safety Regimen Decreases Injuries
- Thurmon E Lockhart, associate professor, Virginia Tech
Inside Science Buzzwords:
- Inner Ear – Of the three sections of the ear, the inner ear is the portion that is involved with both hearing and balance.
- Biomechanics – The study of the forces both inside and outside the body and the effects of these forces on the body.
Science says…Safety first!
http://nationalsciencefoundation.tumblr.com/post/122261940393/science-sayssafety-first
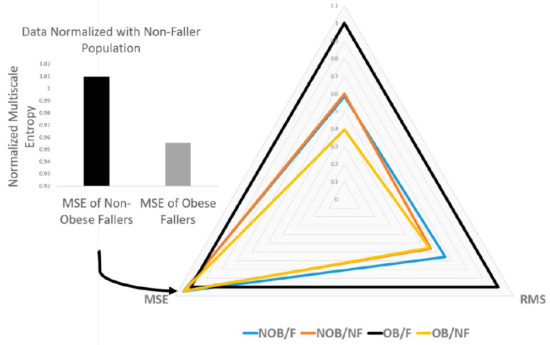
Lockhart Monitor app published
-Assess walking velocity and postural stability with a mobile phone.
-Screenshots of Lockhart monitor.